Amid record STD rates, doctors treat patients' partner's sight unseen
If patients return to Dr. Crystal Bowe soon after taking medication for a sexually transmitted infection, she usually knows the reason: Their partners have re-infected them.
"While you tell people not to have sex until both folks are treated, they just don't wait," she said. "So they are passing the infection back and forth."
That's when Bowe, who practices on both sides of the North and South Carolina border, does something doctors are often reluctant to do: She prescribes the partner's antibiotics without meeting them.
Federal health officials have recommended this practice, known as expedited partner therapy, for chlamydia and gonorrhea since 2006. It allows doctors to prescribe medication to their patients' partners without examining them. The idea is to prevent the kind of reinfections described by Bowe -- and stop the transmission of STDs to others.
However, many physicians aren't taking the federal government's advice because of entrenched ethical and legal concerns.
"Health care providers have a long tradition of being hesitant to prescribe to people they haven't seen," said Edward Hook, a professor at the University of Alabama's medical school in Birmingham. "There is a certain skepticism."
A nationwide surge of sexually transmitted diseases in recent years, however, has created a sense of urgency for doctors to embrace the practice. STD rates have hit an all-time high, according to the Centers for Diseases Control and Prevention.
In 2017, the rate of reported gonorrhea cases increased nearly 19 percent from a year earlier to 555,608. The rate of chlamydia cases rose almost 7 percent to 1.7 million.
"STDs are everywhere," said Dr. Cornelius Jamison, a lecturer at the University of Michigan Medical School. "We have to figure out how to ... prevent the spread of these infections. And it's necessary to be able to treat multiple people at once."
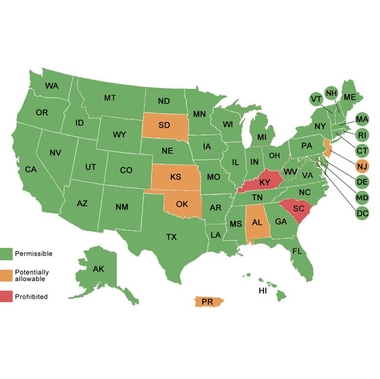
This Expedited Partner Therapy (EPT) is prohibited in two states: South Carolina and Kentucky. In six others it is potentially prohibited; Oklahoma, Kansas, Alabama, New Jersey, South Dakota plus Puerto Rico lack clear guidance for physicians.
The remaining states allow EPT.
Studies show patients were as much as 29 percent less likely to be re-infected when their physicians prescribed medication to their partners. The study also showed that partners who got those prescriptions were more likely to take the drugs than ones who were simply referred to a doctor.
Only about half of providers reported ever having prescribed drugs to the partners of patients with chlamydia, and only 10 percent said they always did so, according to a different study.
Chlamydia rates were higher in states with no law explicitly allowing partner prescriptions; research published earlier this year showed.
Because of increasing antibiotic resistance to gonorrhea, the CDC no longer recommends oral antibiotics alone for the infection. But if patients' partners can't go in for the recommended treatment, which includes an injection, the CDC said that oral antibiotics by themselves are better than no treatment at all.
"Increasing resistance plus increasing disease rates is a recipe for disaster," said David Harvey, executive director of the National Coalition of STD Directors. The partner treatment is important for "combatting the rising rates of gonorrhea in the U.S. before it's too late."
Bowe said that even though she writes STD prescriptions for her patients' partners, she still worries about doing it because of possible drug allergies or side effects.
"I don't know their medical conditions," she said. "I may contribute to a problem down the road that I'm going to be held liable for."
In many cases, doctors and patients simply do not know about partner therapy.
Several medical associations support partner treatment. But they acknowledge the ethical issues, saying it should be used only if the partners are unable or unwilling to come in for care.
Federal officials are trying to raise awareness of the practice by training doctors and other medical professionals, said Laura Bachmann, chief medical officer of the CDC's office of STD prevention. The agency posts a map with details about the practice in each state.
The fact that some states don't allow it, or haven't set clear guidelines for physicians, also creates confusion -- and disparities across state lines.
By Anna Gorman, Kaiser Health News. The-CNN-Wire™ & © 2018 Cable News Network, Inc., a Time Warner Company. All rights reserved.
Copyright The Gayly – December 28, 2018 @7:30 a.m. CST.





