The women’s health issue no one talks about
By Jenny Gold
Kaiser Health News
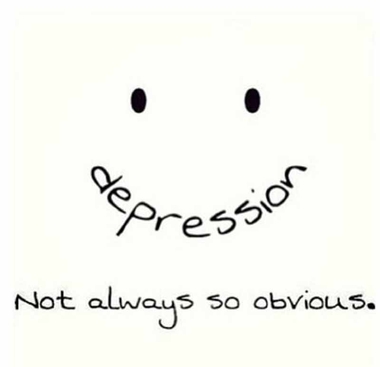
Kieley Parker never imagined she would need an antidepressant. “I always win those stupid sunshine and happiest person awards. People see me as an incredibly joyful person,” she said.
But in fall 2014, Parker left her job as a third-grade teacher and moved to Tulsa, Okla., with her fiancé. Starting over in a new city was an enormous transition. “I couldn’t feel joy or even negative emotions like sadness. I couldn’t eat — I lost 25 pounds,” Parker recalled. “I was just anxious, which spiraled into depression.”
What’s happening
About 1 out of 5 women in America will experience depression in her lifetime, twice the number of men. Some are depressed throughout the course of their lives; others, like Kieley, become depressed following a big change.
Over the past decade, people have increasingly treated depression with medication: Starting in 1994, the number of antidepressant prescriptions written by doctors went up 400 percent over a 10-year period. And today, about 15 percent of women take an antidepressant. Among women age 40 to 59, that number is nearly 23 percent, according to the U.S. Centers for Disease Control and Prevention (CDC).
With so many people popping pills, it’s easy to wonder: Are they being overprescribed? The answer is complicated. “I suspect we have the right number of people taking antidepressants,” said Dr. Karen Swartz, a psychiatrist at Johns Hopkins University School of Medicine in Baltimore. “The question is whether we have the right people taking them.”
One answer could be that some women are incorrectly given antidepressants after brief evaluations with primary care physicians even if they’re not experiencing clinical depression. (Most prescriptions are written by doctors who do not specialize in mental health care.)
Others who may need medication are never diagnosed because they don’t discuss their feelings due to fear of prejudice or lack of access to medical care. And, some women who could benefit from antidepressants may be self-medicating with alcohol instead.
The safety factor
Overall, doctors consider antidepressants a safe treatment. They often bring fast relief, and millions of people have been using them for 30-plus years, without evidence of serious harm, Swartz said. Though research on long-term use is scarce, “generally, studies show that there are no side effects of using antidepressants for an extended duration,” said Dr. Renee Binder, immediate past president of the American Psychiatric Association. However, there can be short-term side effects, including weight gain and insomnia. So “no one wants to be on a medication they don’t need,” Swartz said.
These three women are sharing their stories to spur dialogue around the subject and to encourage others to speak out. Their message: You are not alone.
Barb Patrick, 46, experienced postpartum depression
At least 1 in 7 women suffer from postpartum depression following the birth of a child — Patrick was diagnosed after her second baby in 2000. “I couldn’t sleep at all because of my anxiety. People tell you to relax, but if I could relax, I would!”
Patrick, who now runs a quilting business in Newtown, Conn., worried she couldn’t take care of her newborn and 20-month-old toddler, so she called her OB-GYN office. At first, they didn’t offer any helpful solutions, Patrick said. After five sleepless nights, she called the office again and the on-call nurse midwife answered. “She changed my life. She said, ‘Oh, honey, you have postpartum. Come in, and we’ll take care of it.'” The midwife referred her to a psychiatrist, who put her on Zoloft and Ativan to quell anxiety.
Patrick stopped the medication about a year later, but as soon as she gave birth to her third baby in 2003, the symptoms returned and worsened. She went back on her medications and began to feel better. Since she assumed the depression was specific to childbirth, she tried to go off again several times. On every occasion, the symptoms returned. Today, 13 years later, she remains on antidepressants.
“I had to go through this process to realize this is something I cannot control. My mother said to me, if you had a heart problem, you would take medicine. You can’t control it, so take the medicine. I function perfectly, I have a family and run a business, I have three great kids, I have a house. I manage it all and just accept that medication is part of my life.”
What You Should Know: Some women are able to come off antidepressants when their children get older, while others stay on. “Postpartum depression is often traumatic enough to an entire family that it takes a while for them to even consider going off,” said Swartz.
Tonja Myles, 51, has had multiple depressive episodes
Myles was not dealt an easy hand. She experienced years of childhood trauma and at the age of 18, she was hospitalized for depression and a suicide attempt. She started taking an antidepressant but soon stopped because she felt ashamed. “Some people in the faith community frown upon it because they think you should just pray and ask God, and He will heal you from depression,” said Myles, who is an ordained minister. “I pray, but there are days when I have trouble getting out of bed, and that’s the truth.”
Eventually, at 45, after several episodes of major depression, Myles grew tired of the emotional roller coaster. She went to see a therapist, who recommended again that she take medication. This time, she agreed. “I have to do what’s best for myself,” she said. It took a long time for Myles’ doctor to find the right combination of drugs, but she ended up on a medication called Lexapro, then transitioned to Lamictal (taken as a mood stabilizer) and a pill to help with insomnia. For Myles, taking antidepressants has become a part of her life, along with her faith, exercise, healthy eating and therapy. Today, she counsels others with mental health issues and speaks publicly to reduce prejudice against depression; she also hosts her own community radio show.
What You Should Know: Doctors recommend that women who have three or more episodes of depression stay on antidepressants. “If you stop using antidepressants even after you get well, the risk of relapse is very high — between 50 percent to 75 percent within six months,” said Dr. Lee Cohen, director of the Center for Women’s Mental Health at Massachusetts General Hospital.
Kieley Parker, 30, went through a big life change
When Parker first became ill, even asking for help seemed like more than she could manage. But she gathered her courage and told her mother she was struggling. Right away, her mom was supportive. She scheduled an appointment with a psychiatrist for Parker and drove her there.
Parker, a typically bubbly person, was immediately diagnosed with depression, brought on by her move and all the other transitions in her life. The psychiatrist put her on Zoloft, an antidepressant, and Valium for her anxiety.
“I felt better almost instantly,” she said. “Every day it got a little bit easier and I could feel myself slowly coming back to the person I was before this rocky transition.”
She stayed on antidepressants for two years, as she built her life in Tulsa. Parker tried to go off them briefly, but recently went back on at a lower dose when her anxiety began to creep back in.
What You Should Know: If you were put on antidepressants because of symptoms related to a specific stressor like a divorce and you’re feeling better a year or so later, you can talk to your physician about whether you still need to be on them, said Binder.
Depression vs. Grief: Diagnosing people with depression following a big life event can be tricky because it looks similar to grief, which can include sadness, appetite loss and exhaustion. “An estimated 20 percent of women will have a depressive episode over the course of their lives, but 100 percent will grieve,” said Swartz. “Feeling sad and being tearful is not the same as depression.” The difference: People with depression have a real change in their feelings about themselves and about the future. Depression can also include thoughts of suicide, which is not usually part of grief.
Copyright Henry J. Kaiser Family Foundation. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation. Provided via AP Exchange.
The Gayly – September 19, 2016 @ 4 p.m.





